Peripherally Inserted Central Catheter (PICC Line)
What Are PICC Lines?
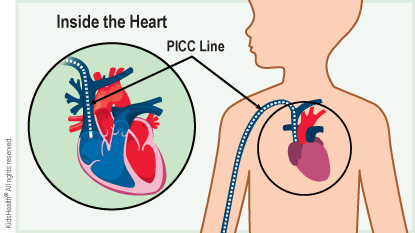
A peripherally inserted central catheter (PICC line) is a type of central line. A central line (also called a central venous catheter) is like an intravenous (IV) line. But it is much longer than a regular IV and goes all the way up to a vein near the heart or just inside the heart. The other end of the PICC line stays outside of the body, usually where the arm bends. It may divide into more than one line. The end of each line is covered with a cap.
A patient can get medicine, fluids, blood, or nutrition through a PICC line. It also can be used to draw blood.
Why Is a PICC Line Used Instead of a Regular IV (Intravenous) Line?
A PICC line is thicker and more durable than a regular IV. It's also much longer and goes farther into the vein. Health care providers use a PICC line instead of a regular IV line because:
- It can stay in place longer (up to 3 months and sometimes a bit more).
- It lowers the number of needle sticks a child needs for blood draws.
- Patients can get large amounts of fluids or medicines (like chemotherapy) that might not go through regular IVs.
A PICC line can help someone:
- with a serious infection so they can get IV for a few weeks
- with cancer so they can get chemotherapy and blood tests through the line
- who needs IV nutrition
- who will need many blood transfusions
What Happens During a PICC Line Placement?
Health care providers place PICC lines in an operating room, intensive care unit, or interventional radiology suite. The patient is sedated (given medicine to relax) or gets general anesthesia (to go to sleep) so they won't feel pain.
To place the line, a health care provider will:
- Clean and numb the skin where the PICC line goes in.
- Put the PICC line into a vein (usually a vein where the arm bends) using ultrasound to guide where the line goes.
- Thread the PICC line up to a large vein near heart.
- Check the placement of the PICC line with an X-ray.
- Place a dressing (bandage) over the PICC line.
Putting in a PICC line takes about 15–20 minutes.
Are There Any Risks to a PICC Line?
Most of the time, there are no problems with a PICC line. If problems do happen, it is usually because the line gets infected or stops working. Very rarely, a PICC line can cause a blood clot. Health care providers review the risks with families before placing the PICC line.
When Should I Call the Health Care Provider?
Check the PICC line area every day and call the health care provider right away if:
- There are signs of an infection, such as a fever, redness or swelling near where the line is, or pain or tenderness where the line is.
- The line comes out or gets blocked (can't be flushed).
Call 911 if your child has trouble breathing, suddenly starts coughing, has chest pain, or their lips or nails look blue.
How Can Parents Help?
At home, a child's PICC line needs special care to prevent infection and keep it working well. It's normal to feel a little bit nervous caring for the PICC line at first, but soon you'll feel more comfortable. You'll get supplies to use at home, and a visiting nurse may come to help you when you first get home.
Before your child goes home, ask your health care team:
- how often to change the dressing
- when and how to flush the line
- what to do if the line gets blocked or comes out
- how to give medicines through the line (if you will be giving medicines at home)
- if the line has caps, how often to change them
- which physical activities are OK for your child (most kids need to avoid rough play and contact sports)
- if any special care is needed to protect the line while your child bathes
- what signs of infection to watch for
Tell your child's teachers, school nurse, counselor, and physical education teacher about the PICC line. They can make sure your child avoids any activities that may damage the line, and help support your child during treatment.


